Hospitals and health systems are facing increased pressure to achieve health equity in the communities they serve.
Corporate social responsibility isn’t a new idea, but the COVID pandemic unmasked the magnitude of long-standing inequities within our communities—the crowded living conditions, homes without plumbing, risks shouldered by low-wage, essential workers, and the fractured broadband infrastructure that exacerbates differences in access to education and health, especially given the sharp pivot to telemedicine.
We have reached a new level of public discourse on the responsibility of the healthcare sector in shaping healthy communities. Despite some pushback about the methodology, when the Lown Institute released their list of America’s most socially responsible hospitals, ten national publications reported on the list. The US News and World Report, in its recent list of America’s Best Hospitals, also ranked hospitals based on health equity. The impulse to prioritize health equity reflects a growing sentiment: health systems around the country are powerful institutions and have the potential to substantially enhance the health outcomes of their communities.
Why should we expect hospitals to address issues beyond the clinical setting?
The issue of social responsibility for hospitals looms large. Many health systems are nonprofit institutions that receive tax exemptions because of their stated commitment to enhancing the health of their communities and the individuals in their service areas. Tax write-offs are an investment from the community - opportunities for neighborhood improvement are diverted when tax collection is limited.
The collective annual tax write-off for non-profit hospitals is $24 billion dollars.
Hospital investment in communities makes financial sense because of a changing Federal policy landscape. 80% of what drives health status is related to factors outside the doctor’s office—where we live, work, worship, and play. The cheapest way to treat a disease is to keep it from happening, but a fee-for-service model disincentivizes this. A transformation to value-based care rewards lower-cost preventative interventions. In recognition of how profoundly community-level factors impact health status, the federal government will no longer reimburse a health system if their cardiac patient must be readmitted from the hospital within 30 days of discharge. Health policy is evolving, and it’s crucial that healthcare providers evolve as well.
The Community Health Needs Assessment provides an opportunity for innovation.
The Federal government realized a discordance in the nonprofit status hospitals enjoy and the level of community benefit they provided before crafting the Affordable Care Act. This legislation prescribed a mandate whereby all private, non-profit hospitals are required to develop a community health needs assessment (CHNA) in coordination with the local health department and community-based organizations. The goal of the CHNA is for health systems to develop and use a dynamic tool to assess, plan, and drive a community health agenda that leads to impactful and sustained change. This is an IRS requirement that must be completed every 3 years, accompanied by a community health improvement plan. If these documents are not submitted, or fail to reach a minimum threshold, these hospitals are fined $50,000.
In my role, I see a lot of CHNA’s from all over the country and, unfortunately, the news isn’t good. There are certainly health systems that have owned their roles as anchor institutions and have exemplary portfolios of substantive community investment. However, for the vast majority, the CHNA process is underutilized and under-resourced.
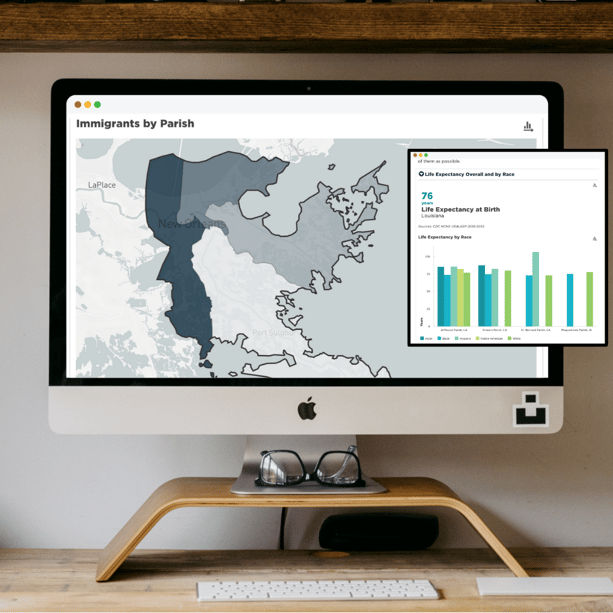
mySidewalk has curated the data to inform your social responsibility and community health investment strategies. mySidewalk's 1.9 billion data points provide the knowledge that health systems need about the communities and neighborhoods they serve in a fraction of the time it would take to acquire and manage this data outside of the system. Our tools allow health systems to easily map data to understand placed-based differences in SDoH and health outcomes. mySidewalk’s data is tailored to understand places and geographies that matter, including service or catchment areas. mySidewalk’s CHNA dashboards are dynamic with up-to-date data, and can easily be adapted as community needs or strategies evolve to ensure stakeholders aren’t behind. These powerful tools facilitate data storytelling so that key audiences come away with a clear understanding of community needs, and so that CHNAs aren’t outdated static documents, but responsive tools for driving change
Putting the “community” back into the CHNA
Health systems around the country should contribute to building the kinds of communities in which we all want to live in by genuinely prioritizing health equity. Society has shifted, and just meeting the minimum requirements to maintain a nonprofit status is not enough. Let’s live up to our commitments to do address health inequities.
Healthcare leaders owe it to their patients and employees to sustain momentum and develop plans and strategies that foster better health outcomes in the communities they serve.
Given what the last two years have revealed, we cannot maintain the status quo. It is time to advance an agenda that capitalizes on cross-sector collaborations, meaningful engagement with our communities, better place-based data, and an openness to learn best practices from the health systems around the country that are already working upstream.
Hospitals are very important members of our communities. In addition to being places where life and death happen, they are economic engines. As I reflect on the lessons from the ongoing pandemic, I’ve realized that communities are only as strong as their weakest members. When we ensure that every community institution is committed to health equity, we will see powerful multiplier effects. There’s an inherent interconnectedness, and our fragile ecosystem only works if we all move forward together.
.png)